D.2: digestion
 image from thinglink.com
image from thinglink.com
In the Digestion Options unit we will expand our knowledge from Topic 6.2 Digestion and Absorption. Our focus will be on the lining of the digestive tract and how the body controls the functions of the digestive system
This unit will last 4 school days
This unit will last 4 school days
Essential idea:
- Digestion is controlled by nervous and hormonal mechanisms.
Nature of science:
- Serendipity and scientific discoveries—the role of gastric acid in digestion was established by William Beaumont while observing the process of digestion in an open wound caused by gunshot. (1.4)
- Describe how William Beaumont was able to determine the role of the stomach in chemical digestion of food.
- Describe how William Beaumont was able to determine the role of the stomach in chemical digestion of food.
Understandings:
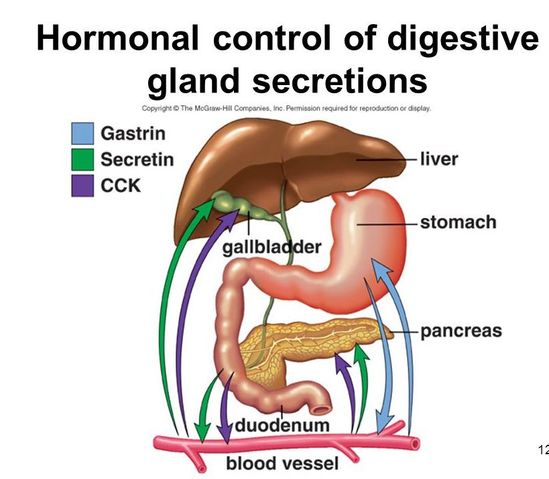
D.2 U 1 Nervous and hormonal mechanisms control the secretion of digestive juices.
- Describe when the secretion of digestive juices must be controlled.
- State to mechanisms by which secretion of gastric juices is controlled.
The secretion of digestive juices is controlled by both nervous and hormonal mechanisms. These mechanisms control both the volume of secretions produced and the specific content (e.g. enzymes, acids, etc.)
Exocrine glands produce and secrete substances via a duct onto an epithelial surface – either:
Examples of digestive glands include:
Exocrine glands produce and secrete substances via a duct onto an epithelial surface – either:
- The surface of the body (e.g. sweat glands, sebaceous glands)
- The lumen of the digestive tract / gut (e.g. digestive glands)
Examples of digestive glands include:
- Sali!ary glands – secrete saliva which contains amylase (breaks down starch).
- Gastric glands – secretes gastric juices which includes %&l acid and proteases (breaks down protein)'.
- Pancreatic glands – secretes pancreatic juices which include lipase,protease and amylase.
- Intestinal glands – secretes intestinal juices via crypts of Liberkuhn in the intestinal wall
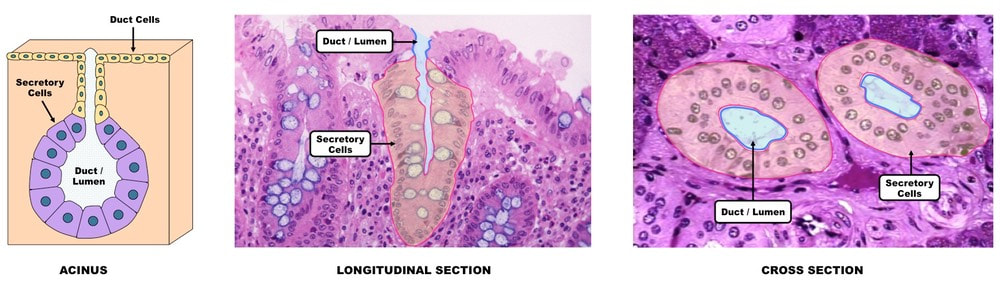
D.2 U 2 Exocrine glands secrete to the surface of the body or the lumen of the gut.
- Define alimentary canal.
- Contrast endocrine glands with exocrine glands.
- Label a diagram of an exocrine gland with the following terms: secretory cells, lumen, duct, secretory vesicles, basement membrane and acinus.
- Discuss the relationship between the structures of an exocrine gland cell and the function of the cell.
- State the name and location of three exocrine glands associated with the alimentary canal.
- State the composition of saliva, gastric juice and pancreatic juice.
The passage through which food passes from mouth to anus is called the alimentary canal. Digestive juices are added to food in the alimentary canal at several points. Exocrine glands secrete juices, including salivary glands, the pancreas, gland cells in the stomach wall and in the wall of the small intestine. The composition of the juices secreted by the glands is different, reflecting the processes that occur in each part of the alimentary canal.
Saliva = salivary glands - water, electrolytes, salivary amylase, mucus, lysozyme
Gastric juice = stomach - water, mucus, enzymes (pepsin), rennin and hydrochloric acid
Pancreatic juice = pancreas - water, bicarbonate, enzymes (amylase, lipase, carboxypeptidase, trypsinogen)
Unlike endocrine glands which secrete directly into the bloodstream, exocrine glands secrete into ducts.
Saliva = salivary glands - water, electrolytes, salivary amylase, mucus, lysozyme
Gastric juice = stomach - water, mucus, enzymes (pepsin), rennin and hydrochloric acid
Pancreatic juice = pancreas - water, bicarbonate, enzymes (amylase, lipase, carboxypeptidase, trypsinogen)
Unlike endocrine glands which secrete directly into the bloodstream, exocrine glands secrete into ducts.
- Exocrine glands have ducts through which they secrete their product (these ducts may arise from the convergence of smaller ductules)
- The ducts / ductules arise from a cluster of cells called an acinus (plural = acini), surrounded by a basement membrane
- Acini are lined by a single layer of secretory cells which release the exocrine product into the lumen of the duct via secretory vesicles
- Secretory cells are held together by tight junctions, and possess a highly developed rough ER and golgi network for material secretion
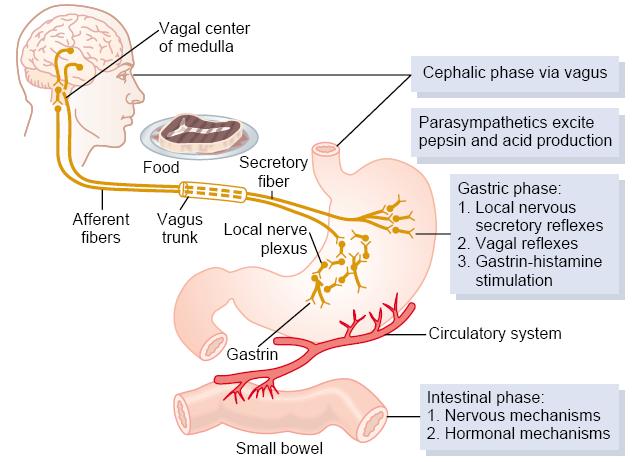
D.2 U 3 The volume and content of gastric secretions are controlled by nervous and hormonal mechanisms.
- Using a flow chart or concept map, diagram the interactions between nervous and hormonal mechanisms that regulated the secretion of gastric juices
Gastric secretion is stimulated and suppressed by nervous and hormonal mechanisms.
Nervous mechanisms
Hormonal mechanisms
Nervous mechanisms
- Involve the Vagus nerve and acetylcholine
Hormonal mechanisms
- Involves gastrin and histamine
- The magnitude of the stimulus results from the additive interactions of acetylcholine, gastrin and histamine
- Low amounts of any one hormone weakly stimulates acid secretion
- Low amounts of all three hormones will strongly stimulate acid secretion
- Somatostatin will suppress acid secretion by blocking the actions of gastrin and histamine
- Acetylcholine, gastrin and histamine stimulate pepisnogen secretion while acetylcholine also stimulates mucous secretion
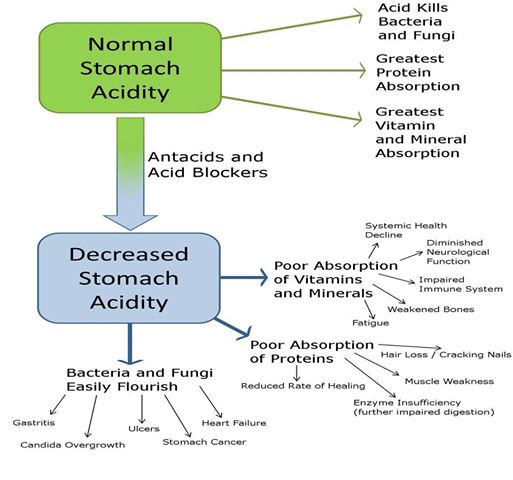
D.2 U 4 Acid conditions in the stomach favour some hydrolysis reactions and help to control pathogens in ingested food.
- Outline three roles of acid in the stomach.
Acid is secreted by the parietal cells of the stomach. The acid disrupts the extracellular matrix that holds cells together in tissues. It also leads to the denaturing of proteins, exposing the polypeptide chains so that the enzyme pepsin can hydrolyse the bonds within the polypeptides. Pepsin is released by chief cells as the inactive pepsinogen. The acid conditions within the stomach convert the inactive pepsinogen to pepsin.. This ensures that the cells that produce pepsinogen are not digested at the same time as the protein in the diet.
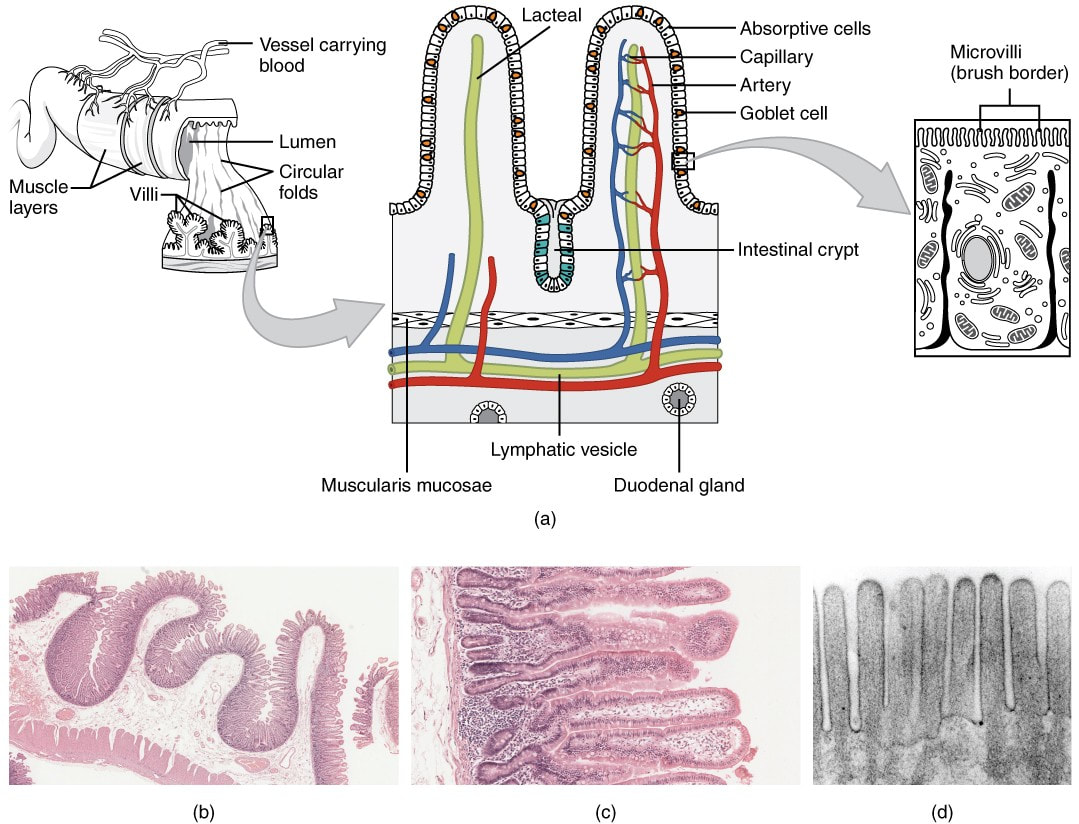
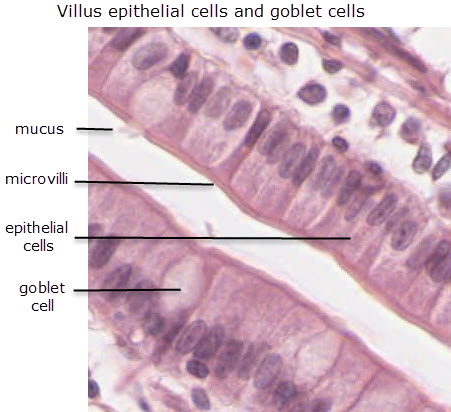
D.2 U 5 The structure of cells of the epithelium of the villi is adapted to the absorption of food
- Outline the role of the following structures of villi epithelial cells: tight junctions, microvilli, mitochondria, pinocytic vesicles, proteins imbedded on the apical surface and proteins imbedded on the basal surface.
The inner surface of the ileum has numerous folds. Each of the folds is covered in tiny projections called villi. Absorption takes place through the epithelial cells covering each villus.
Each epithelial cell covering the villus adheres to its neighbours through tight junctions, which ensure that most materials pass into the blood vessels lining the villi through the epithelial cell. The cell surface membrane on the intestinal lumen side has a number of extensions called microvilli. The collection of microvilli on the intestinal side of the epithelial cells is termed the brush border. The function of the brush border is to increase the surface area for absorption.
Relatively high amounts of ATP are required to drive active transport processes. Thus epithelial cells have large numbers of mitochondria. Pinocytic vesicles are often present in large numbers due to absorption of some foods by endocytosis.
The surface facing the lumen of the intestine is referred to as the apical surface and the surface facing the blood vessels is referred to as the basal surface. These surfaces have different types of proteins involved in material transport.
Each epithelial cell covering the villus adheres to its neighbours through tight junctions, which ensure that most materials pass into the blood vessels lining the villi through the epithelial cell. The cell surface membrane on the intestinal lumen side has a number of extensions called microvilli. The collection of microvilli on the intestinal side of the epithelial cells is termed the brush border. The function of the brush border is to increase the surface area for absorption.
Relatively high amounts of ATP are required to drive active transport processes. Thus epithelial cells have large numbers of mitochondria. Pinocytic vesicles are often present in large numbers due to absorption of some foods by endocytosis.
The surface facing the lumen of the intestine is referred to as the apical surface and the surface facing the blood vessels is referred to as the basal surface. These surfaces have different types of proteins involved in material transport.
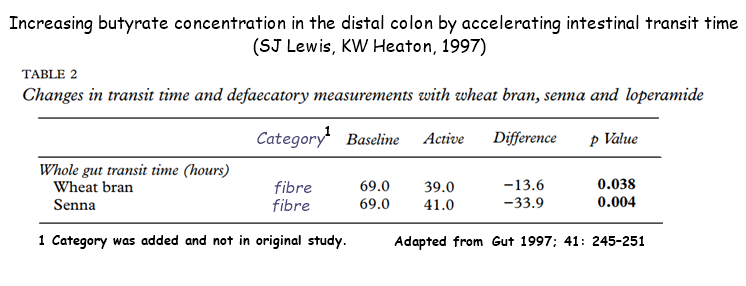
D.2 U 6 The rate of transit of materials through the large intestine is positively correlated with their fibre content.
- List benefits of fibre in a healthy diet.
- State the relationship between food fibre contents and rate of transit through the large intestine.
Dietary fibre is material such as cellulose, lignin and pectin that cannot be readily digested. There are two categories of dietary fibre: soluble and insoluble. A healthy balanced diet contains fibre as it increases the bulk of materials passing through the intestines and helps prevent constipation as it draws water into the intestine. The higher the water content of the intestine, the faster the movement of fecal matter.
There are other possible benefits of fibre in the diet:
There are other possible benefits of fibre in the diet:
- bowel cancer, hemorrhoids and appendicitis risk can be reduced
- the presence of bulky material in the stomach and intestine may increase feelings of satiety, reducing the desire to eat and the risk of obesity
- absorption of sugars may be slowed down, helping to prevent type II diabetes
D.2 U 7 Materials not absorbed are egested.
- Define dietary fibre.
- State two examples of dietary fibre.
- Define egestion.
- List materials that are egested from the body.
Dietary fibre is the edible parts of plants that are resistant to being digested and are not absorbed from the small intestine. Examples include cellulose and lignin. As a consequence, there is a fraction of ingested food which never leaves the digestive tube. In addition, secretion into the digestive tube occurs. Some of what is added is excretory products such as bilirubin from the breakdown of red blood cells. A large volume of water is added to the tube in the process of digestion by secretions in the mouth, stomach and small intestine, and has to be reclaimed in the large intestine. The excretory products, the unabsorbed water and undigested dietary fibre are egested as feces
Applications
D.2 A 1 The reduction of stomach acid secretion by proton pump inhibitor drugs.
- State the role stomach mucus.
- State the cause of ulcer and acid reflux.
- Outline the role of the H+, K+ -ATPase protein pump in the production of an acidic stomach.
- Outline the use, function and effect of proton pump inhibitors to treat gastric disease.
The low pH environment of the stomach is maintained by proton pumps in the parietal cells of the gastric pits. These proton pumps secrete H+ ions (via active transport), which combine with Cl– ions to form hydrochloric acid. Certain medications and disease conditions can increase the secretion of H+ ions, lowering the pH in the stomach.
H+/K+ proton pumps are an integral protein in the cell membrane of parietal cells of the stomach. The proton pump will pump H+ protons from the cell cytoplasm into the stomach lumen and K+ from the lumen into the cell cytoplasm. This involves active transport therefore ATP is required.
Proton pump inhibitors are used to treat gastroesophageal diseases with symptoms of low stomach pH. This is used to promote healing of peptic ulcer diseases or gastroesophageal reflux disease (GERD). Prodrugs bind to the H+/K+ ATPase pump in the apical membrane of the parietal cell irreversibly inhibiting the pumps activity. New proton pumps have to be made in order for acid secretion to resume. the use of these drugs may also encourage the growth of the gut microflora. They may increase the patient's susceptibility to bacterial colonization.
H+/K+ proton pumps are an integral protein in the cell membrane of parietal cells of the stomach. The proton pump will pump H+ protons from the cell cytoplasm into the stomach lumen and K+ from the lumen into the cell cytoplasm. This involves active transport therefore ATP is required.
Proton pump inhibitors are used to treat gastroesophageal diseases with symptoms of low stomach pH. This is used to promote healing of peptic ulcer diseases or gastroesophageal reflux disease (GERD). Prodrugs bind to the H+/K+ ATPase pump in the apical membrane of the parietal cell irreversibly inhibiting the pumps activity. New proton pumps have to be made in order for acid secretion to resume. the use of these drugs may also encourage the growth of the gut microflora. They may increase the patient's susceptibility to bacterial colonization.
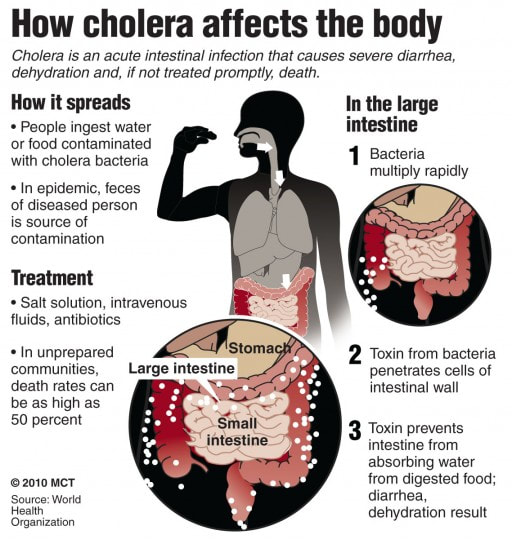
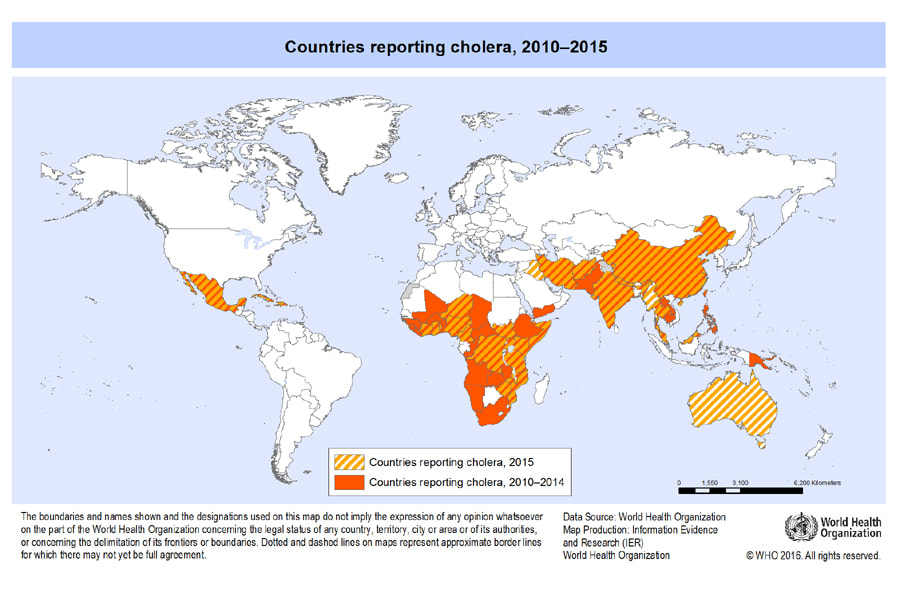
D.2 A 2 Dehydration due to cholera toxin.
- Outline the cause and consequences of cholera infection.
- Explain the effect of cholera toxin on intestinal cells.
Vibrio cholerae is a curved rod bacterium. The pathogen is acquired almost exclusively from drinking water contaminated by feces of patients or carriers of the pathogen
- large numbers of bacteri must be ingested for the disease to develop
- pathogen may survive the stomach acid
- attaches itself to the epithelium membrane
- releases enterotixn.
- toxin triggers loss of ions from the cells
- outflow of water follows
- patient losses a massive amount of body fluid, 15-20 liters may drain from the body as diarrhoea
- death may result from dehydration
- blood circulation collapses
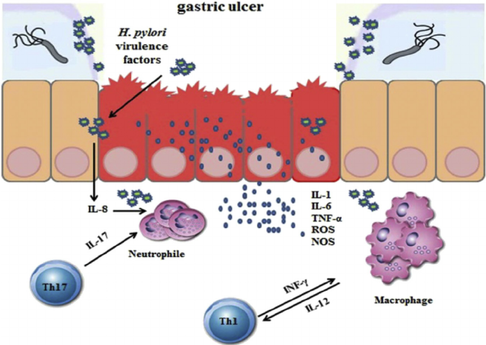
D.2 A 3 Helicobacter pylori infection as a cause of stomach ulcers.
- Define stomach ulcer.
- Outline evidence that suggest Helicobacter pylori infection has a role in stomach ulcer and stomach cancer.
This is an example of a paradigm shift, where existing ideas of scientists and doctors about the tolerance of bacteria to stomach acid were incorrect in spite of the evidence. Australians Robin Warren and Barry Marshall made the discovery of the role of Helicobacter pylori and stomach acid in the formation of ulcers but struggled to convince the scientific and medical community.
Skills
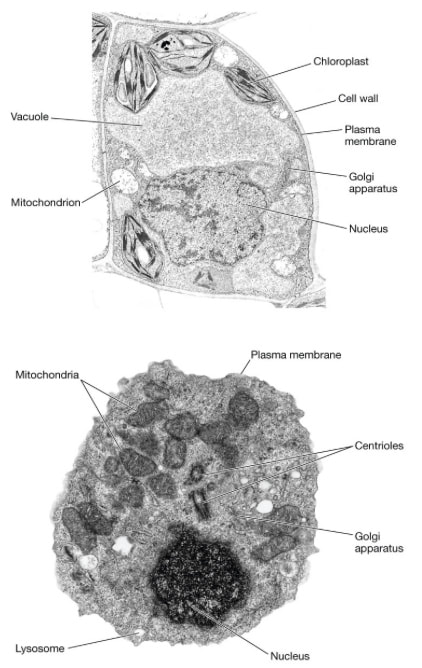
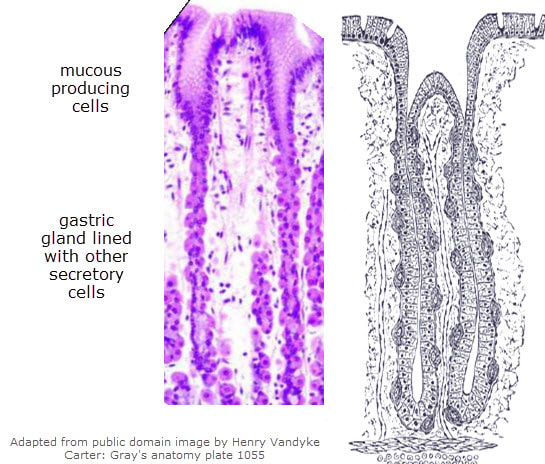
D.2 S 1 Identification of exocrine gland cells that secrete digestive juices and villus epithelium cells that absorb digested foods from electron micrographs.
- List three features that can be used to identify exocrine gland cells as viewed in electron micrographs.
- List four features that can be used to identify villus epithelium cell as viewed in electron micrographs.
Exocrine glands are composed of a cluster of secretor! cells which collectively! form an acinus. The acini are surrounded b! a basement membrane and are held together by tight junctions between secretor! cells.
The secretor! cells possess a highly! developed ER and golgi network for material secretion and are rich in mitochondria.
Exocrine products are released into a duct, which connects to an epithelial surface.
These ducts ma! arise from a convergence of smaller ductules (each connected to an acinus) in order to enhance secretion
The secretor! cells possess a highly! developed ER and golgi network for material secretion and are rich in mitochondria.
Exocrine products are released into a duct, which connects to an epithelial surface.
These ducts ma! arise from a convergence of smaller ductules (each connected to an acinus) in order to enhance secretion
Exocrine Gland
Key Terms
|
digestion
gastric juices alimentary canal secretory vesicles tight junctions basal surface small intestine protein pump dehydration William Beaumont |
ingestion
enzymes endocrine glands basement membrane hormonal mechanisms pinocytic vesicles large intestine stomach mucus cholera somatostatin |
egestion
exocrine glands secretory cells pancreatic juice epithelial cells mitochondria fiber ulcer saliva chemoreceptors |
absorption
lumen acinus nervous mechanisms hydrolysis reactions apical surface constipation acid reflux Helicobacter pylori pepsin |
hormones
gut duct stomach villi microvilli dietary fiber gastric disease secretin |
Classroom Materials
Analyse your lunch with Wolfram|Alpha
Facts About Hunger
Hunger Statistics
Topic D.2 Review
Analyse your lunch with Wolfram|Alpha
Facts About Hunger
Hunger Statistics
Topic D.2 Review
PowerPoint and Notes on Topic D.1 by Christina Reis
Your browser does not support viewing this document. Click here to download the document.
Your browser does not support viewing this document. Click here to download the document.
Correct use of terminology is a key skill in Biology. It is essential to use key terms correctly when communicating your understanding, particularly in assessments. Use the quizlet flashcards or other tools such as learn, scatter, space race, speller and test to help you master the vocabulary.
Useful Links
In The News
Gastric cancer: A new strategy used by Helicobacter pylori to target mitochondria - Science Daily, Nov 2017
Acid reflux drug linked to more than doubled risk of stomach cancer – study - Guardian, Oct 2017
Tuning the Tide Against Cholera - New York Times, Feb 2017
Video Clips
An unfortunate accident in June 1822 led to a real breakthrough in the understanding of how the digestive system, and particularly the stomach, works.
The Journey of the Digestive System'
If you're like us, you love the sound of a brunch buffet. But not everything you eat at that glorious buffet is going to be turned into energy. Your body has to work with different forms of food in different ways. In this episode of Crash Course Anatomy & Physiology, Hank takes us through more about our metabolism including cellular respiration, atp, glycogenesis, and how insulin regulates our blood sugar levels.
Nachos are great...if you are among the lucky ones whose body can digest them. When digestion goes according to plan, the small intestine performs most of your chemical digestion in the duodenum, while accessory organs including the liver, gallbladder, and pancreas contribute enzymes that all but finish the job. Then your large intestine, which is actually shorter than the small intestine, tries to extract the last bit of nutrition, including the occasional attempt to turn nachos into energy, which for most humans, ends in gassy failure
Ted Ed How The Digestive System Works
Hormonal Regulation of the Secretion of Acids in the Stomach
Learn the basics about what stomach acid is as part of the acids and bases topic.
The Villi
What Causes Constipation
The following animation details the mechanism of action of proton pump inhibitors (PPIs)
Cholera is an aggressive bacterial infection that can kill its victims within hours, but how? What exactly does cholera do to our bodies?
Describes in detail and concisely the pathogenesis of helicobacter pylori infection.