D.4: Function of the heart

In the Functions of the Heart unit is an extension of Topic 6.2 The Blood System. However, the emphasis will be on the function and structure of the heart. We will learn how electrical impulses sent from the brain regulate the heart beat and how this can measured. We will also look at factors that can affect the function of the heart.
This unit will last 4 school days.
This unit will last 4 school days.
Essential idea:
- Internal and external factors influence heart function.
Nature of science:
- Developments in scientific research followed improvements in apparatus or instrumentation—the invention of the stethoscope led to improved knowledge of the workings of the heart. (1.8)
- List variables that lead to the development of the stethoscope.
- State the function of the stethoscope.
Understandings:
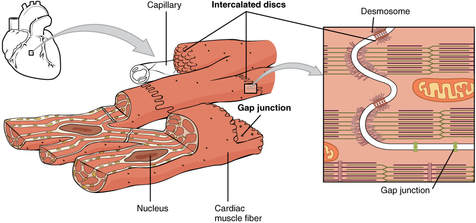
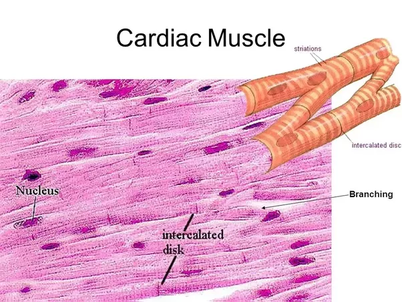
D.4 U 1 Structure of cardiac muscle cells allows propagation of stimuli through the heart wall.
- Compare cardiac muscle tissue to skeletal muscle tissue.
- Contrast cardiac muscle tissue to skeletal muscle tissue.
- Describe how the Y-shape, intercalated discs and gap junctions of cardiac muscle cells allow for propagation of the stimulus to contract.
Cardiac muscle tissue is unique to heart. It is striated in appearance and contractile proteins actin and myosin is similar to that of skeletal muscles. Cardiac muscles are shorter and wider than skeletal and have only one nucleus where skeletal has many.
Contraction of cardiac is not voluntary.
Cells are Y-shaped and join end to end in a network of interconnections. When two cell ends meet they are connected by a specialized junction called an intercalated disc (only in cardiac cells). The disc consist of a double membrane containing gap junctions that provide channels of connected cytoplasm between the cells. This allows rapid movement of ions and low electrical resistance. The Y shape and being electrically connected by gap junctions allows a wave of depolarization to pass easily from one cell to a network of other cells and a synchronization of contraction. So heart contracts as one large cell.
Lots of mitochondria found in cells to supply energy.
Contraction of cardiac is not voluntary.
Cells are Y-shaped and join end to end in a network of interconnections. When two cell ends meet they are connected by a specialized junction called an intercalated disc (only in cardiac cells). The disc consist of a double membrane containing gap junctions that provide channels of connected cytoplasm between the cells. This allows rapid movement of ions and low electrical resistance. The Y shape and being electrically connected by gap junctions allows a wave of depolarization to pass easily from one cell to a network of other cells and a synchronization of contraction. So heart contracts as one large cell.
Lots of mitochondria found in cells to supply energy.
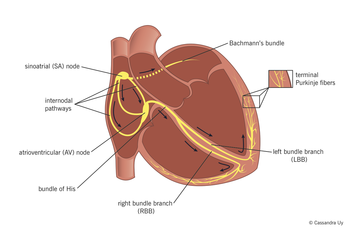
D.4 U 2 Signals from the sinoatrial node that cause contraction cannot pass directly from atria to ventricles.
- Explain the events of the cardiac cycle, including atrial and ventricular systole and diastole and the movement of the signal to contract through the heart.
- Outline the role of the atrioventricular node in the cardiac cycle.
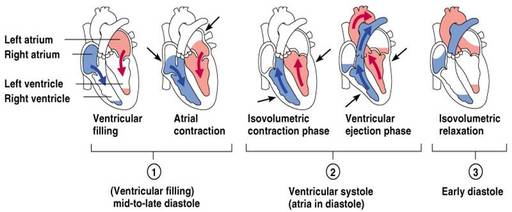
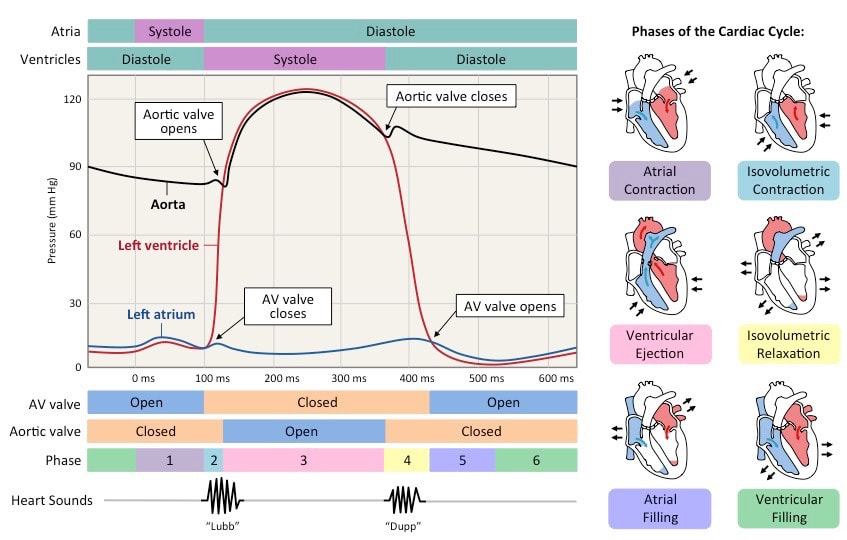
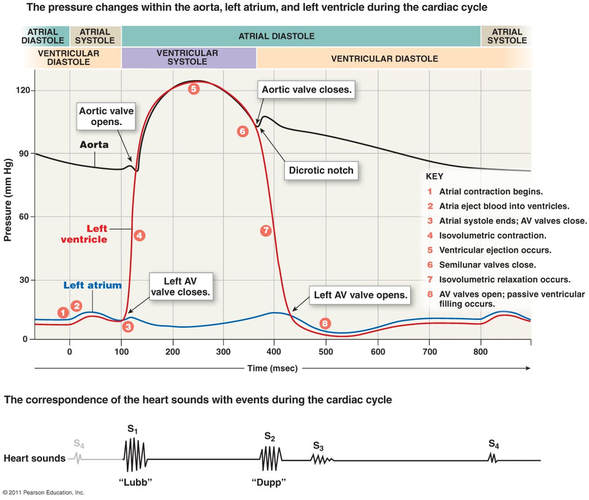
Cardiac cycles is a repeating sequence of actions in the heart that result in pumping of blood to lungs and body. Cycle starts with beginning of one heartbeat to the beginning of next. Contraction of heart’s chambers is systole and relaxation is diastole.
D.4 U 3 There is a delay between the arrival and passing on of a stimulus at the atrioventricular node.
- Outline the causes of the delayed initiation of contraction of ventricles.
The contractions of the atria and ventricles must be staggered so blood flows in the correct direction. When action potential is delayed about 0.12 seconds. Action potential starts at SA node and travels to the AV node. The fibers in the AV node take longer to become excited.
Reasons why: They have smaller diameter and don’t conduct as quickly, reduced number of Na+ channels in membranes, fewer gap junctions between cells, more non-conductive connective tissue in node.
Reasons why: They have smaller diameter and don’t conduct as quickly, reduced number of Na+ channels in membranes, fewer gap junctions between cells, more non-conductive connective tissue in node.
D.4 U 4 This delay allows time for atrial systole before the atrioventricular valves close.
- State the function of a delayed contraction of the ventricle.
The delay allows atria to contract and empty blood into ventricles before the ventricles contract. It this didn’t happen the ventricles would contract at the same time pushing blood back into atrium and a small volume of blood being moved into ventricles.
D.4 U 5 Conducting fibres ensure coordinated contraction of the entire ventricle wall.
- Describe the motion of the signal to contract from the AV node through the ventricles.
- List features of Purkinje fibers that facilitate rapid conduction of the contraction signal through the ventricle.
- State that the contraction of the ventricle begins at the heart apex.
- Once through the AV node and bundle, the signal is conducted rapidly to ensure the coordinated contraction of the ventricles.
- The signal moves down fibers that split into the right and left bundle branches and these branches conduct the impulse through the walls of the two ventricles.
- At the base or apex of the hear the bundles connect to Purkinje fibers which conduce the signal even more rapidly to the ventricles. The Purkinje fibers have modifications that help conduct at high speeds: have fewer myofibrils, bigger diameter, more voltage-gated sodium channels, and lots of mitochondria.
- Contraction of ventricles begins at the apex of heart.
D.4 U 6 Normal heart sounds are caused by the atrioventricular valves and semilunar valves closing causing changes in blood flow.
- State the cause of each of the two sounds of the heartbeat.
A normal heartbeat has two sounds, both caused by the closing of valves:
- Atrioventricular valves snap shut there is a “lub” sound
- Semilunar valve shut there is a “dub” sound
Application
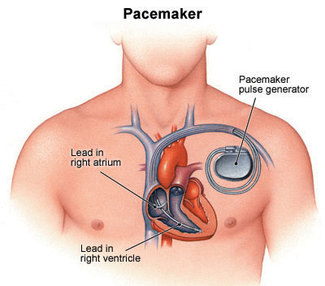
D.4 A 1 Use of artificial pacemakers to regulate the heart rate.
- State the purpose of an artificial pacemaker device
Pacemakers are medical devices that are surgically fitted in patients with malfunctioning sinoatrial node. The devices maintains the rhythmic nature of the heartbeat. They can provide a regular impulse or discharge only when heartbeat is missed so that it beats normally. Most common is the one that monitors heartbeat and initiates one if a beat is missed. The ventricle is stimulated with a low voltage pulse.
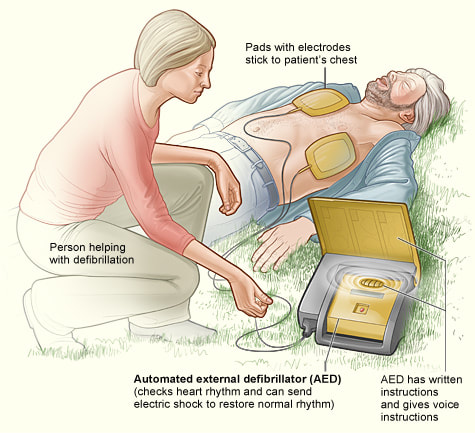
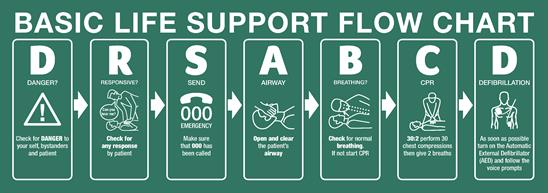
D.4 A 2 Use of defibrillation to treat life-threatening cardiac conditions.
- State the cause and effect of ventricular fibrillation.
- State the purpose of a defibrillator.
Cardiac arrest occurs when blood supply to hear is reduced and heart tissues are deprived of oxygen. First negative consequences of abnormalities in cardiac cycles is ventricular fibrillation or twitching of ventricles due to rapid and chaotic contractions.
Defibrillation is a technique used in emergency medicine to terminate ventricular fibrillation or pulseless ventricular tachycardia. It uses an electrical shock to reset the electrical state of the heart so that it may beat to a rhythm controlled by its own natural pacemaker cells. It is not effective for asystole (complete cessation of cardiac activity, more commonly known as "flatline") and pulseless electrical activity (PEA).
The purpose of defibrillation of ventricular arrhythmias is to apply a controlled electrical shock to the heart, which leads to depolarization of the entire electrical conduction system of the heart. When the heart repolarizes, the normal electrical conduction may assert itself, in which case the ventricular arrhythmia is terminated.
However, if not enough energy is used for defibrillation, the heart may not be completely depolarized, in which case the ventricular tachycardia or fibrillation may not be terminated. Also, if the heart itself is not getting enough oxygen or if there is an instability of the electrolytes in the cardiac cells, the ventricular arrhythmia may recur.
Defibrillation is a technique used in emergency medicine to terminate ventricular fibrillation or pulseless ventricular tachycardia. It uses an electrical shock to reset the electrical state of the heart so that it may beat to a rhythm controlled by its own natural pacemaker cells. It is not effective for asystole (complete cessation of cardiac activity, more commonly known as "flatline") and pulseless electrical activity (PEA).
The purpose of defibrillation of ventricular arrhythmias is to apply a controlled electrical shock to the heart, which leads to depolarization of the entire electrical conduction system of the heart. When the heart repolarizes, the normal electrical conduction may assert itself, in which case the ventricular arrhythmia is terminated.
However, if not enough energy is used for defibrillation, the heart may not be completely depolarized, in which case the ventricular tachycardia or fibrillation may not be terminated. Also, if the heart itself is not getting enough oxygen or if there is an instability of the electrolytes in the cardiac cells, the ventricular arrhythmia may recur.
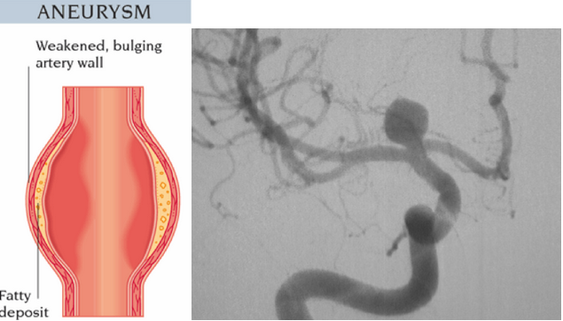
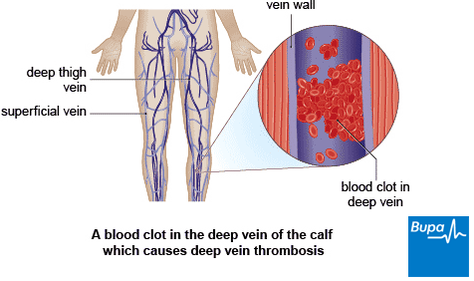
D.4 U 3 Causes and consequences of hypertension and thrombosis.
- Describe the relationship between atherosclerosis and thrombosis.
- Describe the relationship between atherosclerosis and hypertension.
- List consequences of hypertension.
- Outline factors that are correlated with a greater incidence of thrombosis and hypertension.
Atherosclerosis
Thrombosis
The formation of clots inside blood vessels. The incidence of thrombosis is correlated with
- Hardening of arteries caused by formation of plaques on inner lining of arteries.
- Plaques are swollen areas and accumulate debris.
- Develops because of high circulating levels of lipids and cholesterol reducing the speed of which blood moves through vessels.
- Triggers a clot, or thrombosis, which can block blood flow in that artery and deny the tissue access to oxygen.
- If this occurs on surface of heart it can cause a heart attack (myocardial infarction)
- Greater pressure on walls of arteries caused by slowed blood flow.
- Damage to cells that line arteries causing artery to become narrower and stiff,
- Constant high blood pressure can weaken artery causing wall to enlarge and form bulge (aneurysm) that can bust and cause internal bleeding, chronic high blood pressure that can lead to stroke by weakening blood vessels in brain, chronic high blood pressure causes kidney failure.
Thrombosis
The formation of clots inside blood vessels. The incidence of thrombosis is correlated with
- Eating excessive amounts of saturated fats and cholesterol promotes plaque formation
- Sedentary lifestyles and obesity promote plaque formation
- Genetic predisposition e.g high cholesterol production to these conditions
- Old age leading to less flexibility in the walls of blood vessels
- Gender - males are at higher risk possible due to lower oestrogen levels
- Nicotine in cigarette smoke causes vasoconstriction which can increase the chances of clot formation
- Excessive amounts of alcohol
- Stress increases blood pressure and hence the chance of plaque rupture
Skills
D.4.S 1 Measurement and interpretation of the heart rate under different conditions.
- List variables that can influence heart rate.
- Outline methods for detecting heart rate.
- Different variables can influence heart rate.
- Exercise, intensity of exercise, recovery from exercise, relaxation, body position including lying down, breathing, and breath holding, exposure to a cold stimulus, and facial immersion in water all affect heart rate.
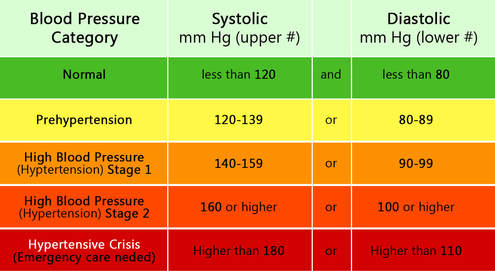
D.4 S 2 Interpretation of systolic and diastolic blood pressure measurements.
- State the cause of systolic and diastolic pressure.
- Describe how sound is used to measure blood pressure.
- Blood pressure or arterial pressure is the pressure that circulating blood puts on the walls of the arteries. Peak pressure occurs during ventricle systole to a minimum near beginning of the cardiac cycle when ventricles are filled with blood and are in systole.
- Measurement in pressure units “mmHg” Example is 120 over 80. Higher number is the pressure in the artery caused by ventricular systole and lower number refers to pressure in artery due to ventricular diastole
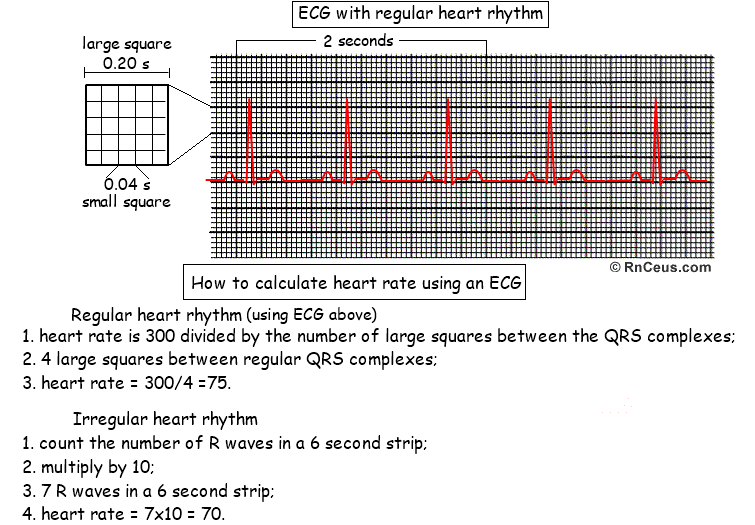
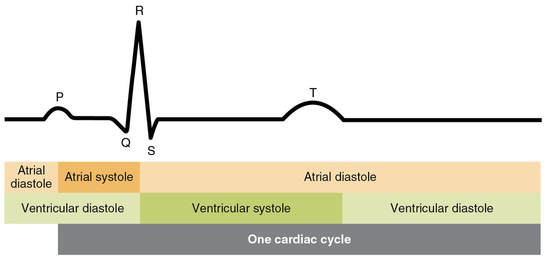
D.4 S 3 Mapping of the cardiac cycle to a normal ECG trace.
- State the function of an electrocardiogram.
- Label the P, Q, R, S and T waves on an ECG trace.
- State the cause of the P wave, the QRS wave and the T wave.
- State an application of the use of ECG technology.
Cardiac muscle contracts because it receives electrical signals. These signals can be detected by electrocardiogram (EKG)
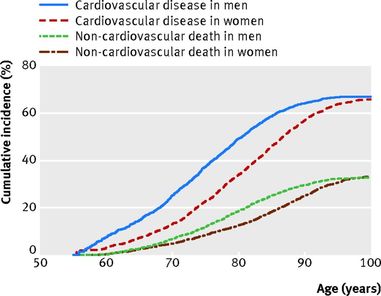
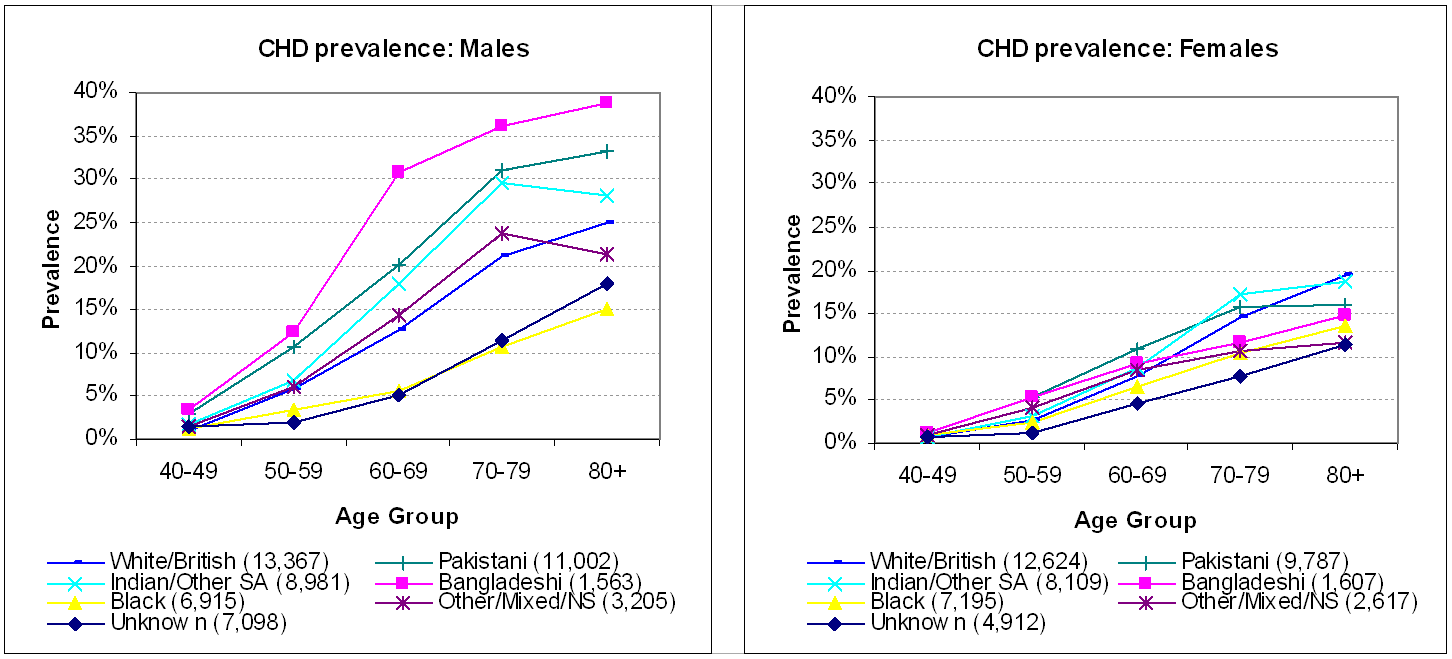
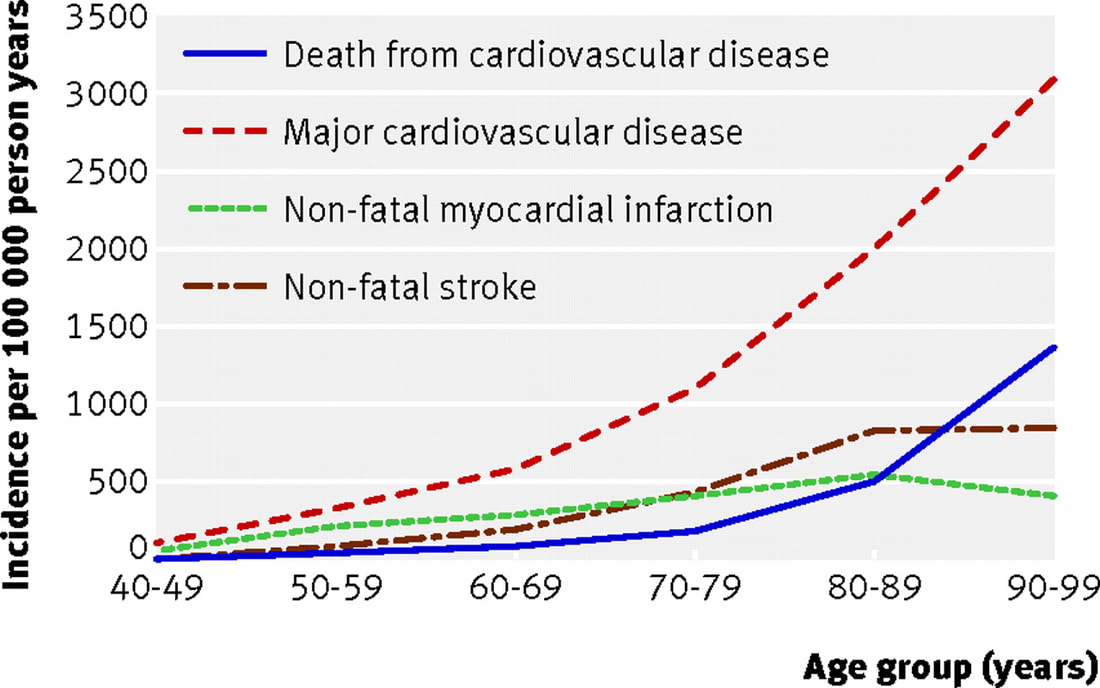
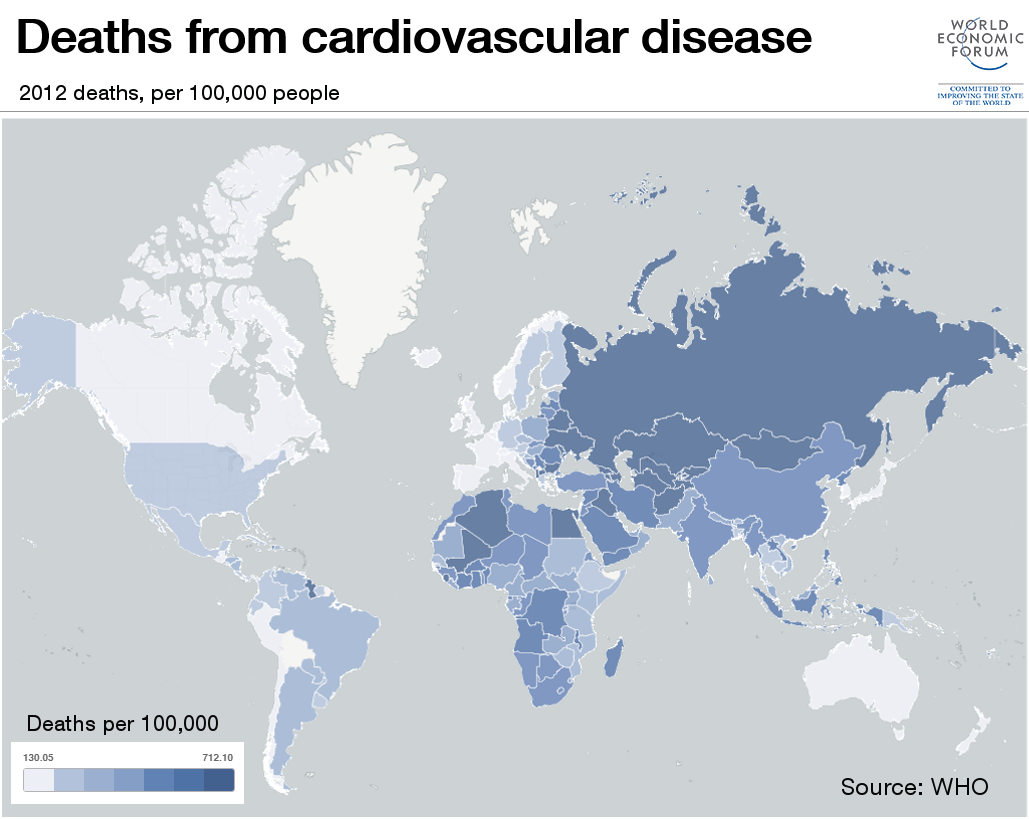
D.4 S 4 Analysis of epidemiological data relating to the incidence of coronary heart disease.
- Define epidemiology.
- List epidemiological factors that can predispose ethnic groups to coronary heart disease.
Coronary heart disease refers to the damage to the heart as a consequence of reduced blood supply to the tissues of the heart itself. Often caused by narrowing and hardening of the coronary artery. Epidemiology is the study of the patterns, causes and effects of diseases in groups of individuals or populations.
Ethic groups can differ in their disposition of CHD because of differing diets and lifestyles. Gender groups, age groups, groups that differ in level of physical activity can also differ.
Ethic groups can differ in their disposition of CHD because of differing diets and lifestyles. Gender groups, age groups, groups that differ in level of physical activity can also differ.
Use graph above to make conclusions regarding CHD Mortality in men and women
Use graph above to make conclusions regarding CHD Mortality in different ethnic groups
- CHD mortality increased with age in all countries
- CHD mortality is greater in males than females at each age
- Greater difference in CHD mortality in elderly between countries in males and females.
Use graph above to make conclusions regarding CHD Mortality in different age groups
Key Terms
|
cardiac muscle tissue
Y-shape atria delayed initiation atrioventricular valves hypertension diastolic pressure stethoscope myofibrils |
propagation
intercalated discs ventricle Purkinje fibers heart beat thrombosis electrocardiogram myosin sodium channels |
stimulus
gap junctions systole heart apex defibrillation heart rate epidemiology actin |
skeletal muscle tissue
sinoatrial node diastole atrioventricular node semilunar valves ventricular fibrillation P, Q, R, S, T waves sarcolemma |
heart wall
cardiac cycle atrial systole artificial pacemakers atherosclerosis systolic pressure heart disease desosomes |
Your browser does not support viewing this document. Click here to download the document.
Your browser does not support viewing this document. Click here to download the document.
Correct use of terminology is a key skill in Biology. It is essential to use key terms correctly when communicating your understanding, particularly in assessments. Use the quizlet flashcards or other tools such as learn, scatter, space race, speller and test to help you master the vocabulary.
Useful Links
TOK
- Symbols are used as a form of non-verbal communication. Why is the heart used as a symbol for love? What is the importance of symbols in different areas of knowledge?
Video Clips
In this medical animation we take a look at the heart and how it pushes oxygenated blood out to the body then returns to be re-oxygenated by the lungs and pushed out again.
Electrical Conduction System of the Heart (cardiac conduction system): This video explains how the SA node, AV node, bundle of His, right and left bundle branch, and purkinje fibers allow the heart to contract which causes the PQRST wave you see on an EKG. (note the test questions are not IB questions)
Phases of the cardiac cycle.
The stethoscope is the single most widely used medical instrument in the world. But where did the idea come from? In the seventh installment of our ‘Moments of Vision’ series, Jessica Oreck shares the modest origins of this incredibly useful item.
A Brief animation about what a Defibrilator is and how it works
What is electrocardiography (ECG/EKG). ECG is a way to measure the electrical activity of the heart.
AED's, or Automatic External Defibrillators increase the chance of survival of a heart attack victim by 90%.
This educative cartoon shows what any patient or family member should understand about cardiovascular disease, when confronted with a diagnosis of carotid artery stenosis, abdominal aneurysm or claudication.
Approximately seven million people around the world die from heart attacks every year. And cardiovascular disease, which causes heart attacks and other problems like strokes, is the world’s leading killer. So what causes a heart attack?