topic 6.2: the blood system
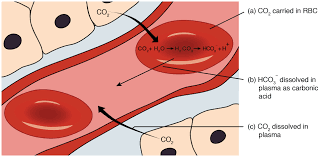 image from BC Open Textbooks
image from BC Open Textbooks
In the Blood System unit we we learn about how our blood system provides a delivery and collection service for the whole body. The heart, blood and blood vessels make up a most efficient transport system that reaches all cells, bringing the substances they need and taking away their waste. You will also learn that humans and other mammals have what is known as a closed circulatory system with blood contained inside a network of arteries, veins and capillaries.
This unit will last 4 school days
This unit will last 4 school days
Essential idea:
- The blood system continuously transports substances to cells and simultaneously collects waste products.
Nature of science:
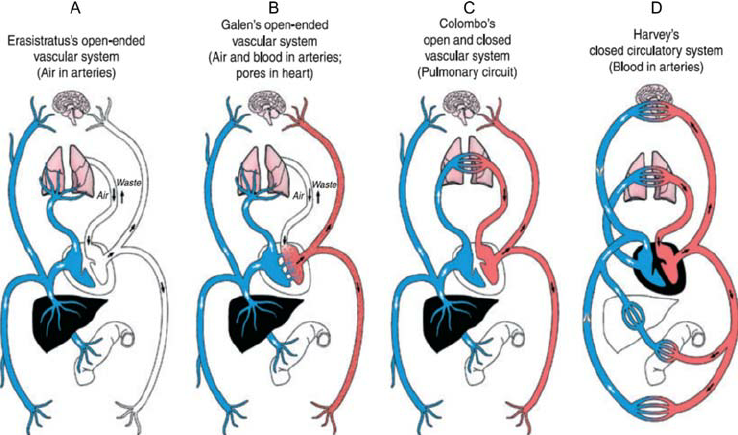
- Theories are regarded as uncertain—William Harvey overturned theories developed by the ancient Greek philosopher Galen on movement of blood in the body. (1.9)
- Outline Galen’s description of blood flow in the body.
- Describe how Harvey was able to disprove Galen’s theory.
Understandings:
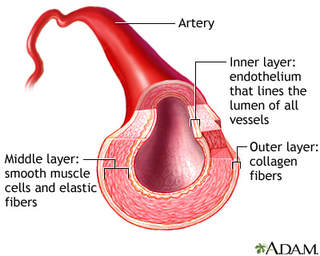
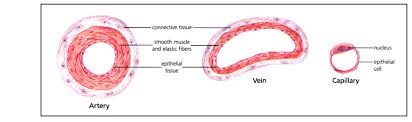
6.2.U1 Arteries convey blood at high pressure from the ventricles to the tissues of the body. (Oxford Biology Course Companion page 291)
- State the function of arteries.
- Outline the role of elastic and muscle tissue in arteries.
- State the reason for toughness of artery walls.
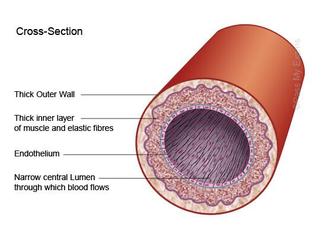
The function of arteries is to convey blood at high pressure from the heart ventricles to the tissues of the body and lungs. Because large volumes of blood are flowing directly out of the heart, arteries must be able to withstand the high pressure and high blood volume created when the ventricles contract. Arteries have a specialised structure in order to accomplish this task:
- They have a narrow lumen (relative to wall thickness) to maintain a high blood pressure (~ 80 – 120 mmHg)
- They have a thick wall containing an outer layer of collagen to prevent the artery from rupturing under the high pressure
- Very thick wall of smooth muscle tissue surrounding arteries makes them strong and elastic in nature with a narrow lumen (area where the blood flows).
- Elastin fibres store energy when they are stretched by the flow of blood. As they recoil the blood is further propelled through the artery.
- The thick smooth muscle layer in the arteries can be used to help regulate blood pressure by changing the diameter of the arteries.
6.2.U2 Arteries have muscle cells and elastic fibres in their walls. (Oxford Biology Course Companion page 291)
- Describe the structure and function of the three layers of artery wall tissue.
Tunica externa – outer layer made from connective tissue
Tunica media– thick layer containing smooth muscle and elastin fibres
Tunica intima– endothelium layer that lines the inside of the artery
Tunica media– thick layer containing smooth muscle and elastin fibres
Tunica intima– endothelium layer that lines the inside of the artery
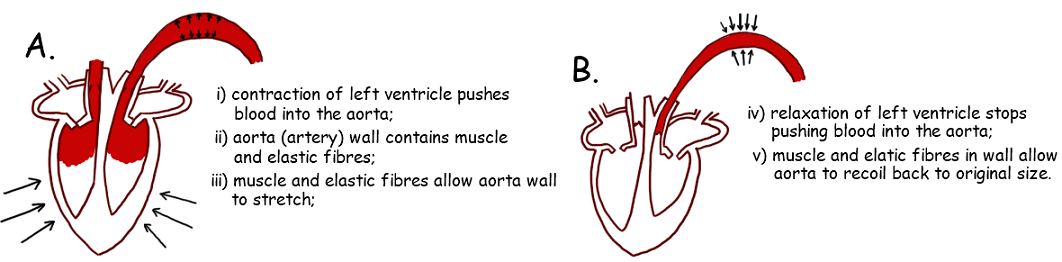
6.2.U3 The muscle and elastic fibres assist in maintaining blood pressure between pump cycles. (Oxford Biology Course Companion page 292).
- Describe the mechanism used to maintain blood flow in arteries between heartbeats.
- Define systolic and diastolic blood pressure.
- Define vasoconstriction and vasodilation.
Blood is expelled from the heart upon ventricular contraction and flows through the arteries in repeated surges called pulses. This blood flows at a high pressure and the muscle and elastic fibres assist in maintaining this pressure between pumps
When the ventricles of the heart contract (systole), the blood leaves the heart through the arteries at a very high pressure.
- The muscle fibres help to form a rigid arterial wall that is capable of withstanding the high blood pressure without rupturing. Muscle fibres can also contract to narrow the lumen, which increases the pressure between pumps and helps to maintain blood pressure throughout the cardiac cycle
- The elastic fibres allow the arterial wall to stretch and expand upon the flow of a pulse through the lumen. The pressure exerted on the arterial wall is returned to the blood when the artery returns to its normal size (elastic recoil). The elastic recoil helps to push the blood forward through the artery as well as maintain arterial pressure between pump cycles
When the ventricles of the heart contract (systole), the blood leaves the heart through the arteries at a very high pressure.
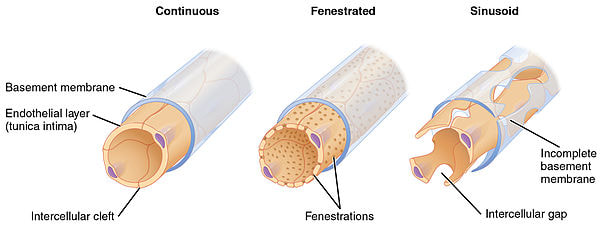
6.2.U4 Blood flows through tissues in capillaries. Capillaries have permeable walls that allow exchange of materials between cells in the tissue and the blood in the capillary. (Oxford Biology Course Companion page 293)
- Describe the structure and function of capillaries.
- Describe the cause and effect of diffusion of blood plasma into and out of a capillary network.
The function of capillaries is to exchange materials between the cells in tissues and blood travelling at low pressure (<10mmHg):
- Capillaries have a very narrow diameter (10 µm) with thin surrounding endothelium cells to allow the shortest distance for O2 to diffuse into the blood from the alveoli in the lungs and from the blood into the body tissues. CO2 also can easily diffuse out of the blood into the alveoli in the lungs and from the tissue into the blood after respiration.
- The walls have pores, making them very permeable allowing plasma to leak out and form tissue fluid, which contains oxygen, glucose and all other substances contained in the blood plasma, except proteins (too large to fit through the pores in the capillary wall)
- Highly branched networks of capillaries increase the surface area, maximizing the amount of nutrients and gases that can move in and out of the capillaries.
- Because they are highly branched, the blood slows down to allow efficient transfer of O2 and CO2 into and out of the capillaries.
- Below are examples what capillaries look like. The pores or holes that allow certain substances to leave get larger from left to right, with Sinusoid capillaries having the largest openings. Specific names of these types of capillaries is not required.
Capillaries structure may vary depending on its location in the body and specific role:
- The capillary wall may be continuous with endothelial cells held together by tight junctions to limit permeability of large molecules
- In tissues specialised for absorption (e.g. intestines, kidneys), the capillary wall may be fenestrated (contains pores)
- Some capillaries are sinusoidal and have open spaces between cells and be permeable to large molcules and cells (e.g. in liver)
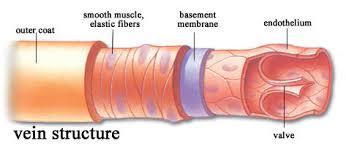
6.2.U5 Veins collect blood at low pressure from the tissues of the body and return it to the atria of the heart. (Oxford Biology Course Companion page 293)
- State the function of veins.
- Outline the roles of gravity and skeletal muscle pressure in maintaining flow of blood through a vein.
The function of veins is to collect the blood from the tissues and convey it at low pressure to the atria of the heart:
- Transport blood back to the heart from the capillary beds in tissues.
- Very low blood pressure and therefore the walls can be thin. Blood is pushed back to the heart through the contraction of skeletal muscles. As the muscles contract, the veins are squeezed, pushing the blood back towards the heart
- Large lumen allows large amounts of blood to slowly return to the heart because the blood has to slow down as it passes through the capillary beds.
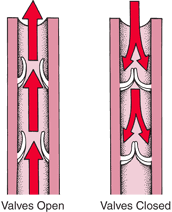
6.2.U6 Valves in veins and the heart ensure circulation of blood by preventing backflow. (Oxford Biology Course Companion page 294).
- Outline the structure and function of a pocket valve.
Since the blood pressure in the veins is quite low because the blood slows down considerably when it reaches the capillary bed and there is not another pump like the heart to speed up the flow and increase the pressure, veins have a series of valves to prevent backflow.
- Valves are flaps of tissue that form pockets to prevent blood from flowing backwards in the wrong direction
- If the blood starts to flow backwards, it gets caught in the pocket valves causing that section of the vein to fill.
- When another contraction occurs and the blood starts to flow in the correct direction, the valves open allowing the blood to continue its movement towards the heart.
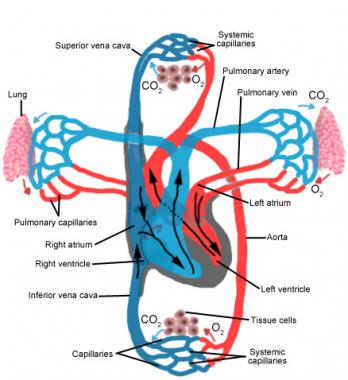
6.2.U7 There is a separate circulation for the lungs. (Oxford Biology Course Companion page 294).
- Draw a diagram to illustrate the double circulation system in mammals.
- Compare the circulation of blood in fish to that of mammals.
- Explain the flow of blood through the pulmonary and systemic circulations.
- Explain why the mammalian heart must function as a double pump.
Humans and other mammals have a two different circulations of blood (blood is pumped twice). One circulation (systemic circulation) goes from the left ventricle to the rest of the body and back to the right atrium. The second circulation (pulmonary circulation) goes from the right ventricle to the lungs and returns to the left atrium of the heart.
Pulmonary Circulation
Systemic Circulation
Pulmonary Circulation
- Blood flows from the right atrium into the right ventricle through the R.atrio-ventricular valve. The right atrium contracts right when the ventricle is almost full in order to push the rest of the blood into the ventricle.
- The right ventricle contracts sending the blood out of the ventricle (past a semi-lunar valve), through the pulmonary arteries to the lungs.
- The atrio-ventricular valve shuts preventing back flow into the atrium.
- The blood flows through capillaries obtaining oxygen from the lungs and returning to the heart by the pulmonary veins; which empty into the left atrium.
- This blood is actually returning to the heart from the lungs at the same time as the blood that returns to the right atrium from the rest of the body.
Systemic Circulation
- The blood then flows into the left ventricle through an L atrio-ventricular valve.
- The left ventricle contracts, sending the blood through another semi-lunar valve and out through the biggest artery in the body called the aorta.
- Again the atrio-ventricular valve shuts, preventing backflow into the atrium.
- The oxygenated blood flows to all the tissues and organs in the body to be used in aerobic respiration. (Arteries --> Arterioles --> Capillaries)
- Blood then flows from the capillaries to the numerous venules and then through the different veins in the body
- These will all eventually dump the blood into the inferior and superior vena cava
- Blood returns to the right atrium of the heart flowing from the inferior vena cava (blood from lower body) and the superior vena cava (blood coming upper body and head).
- Note: Both ventricles contract at the same time sending blood to the lungs and the other parts of the body.
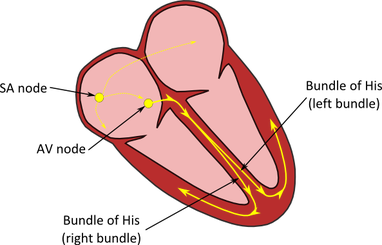
6.2.U8 The heartbeat is initiated by a group of specialized muscle cells in the right atrium called the sinoatrial node. (Oxford Biology Course Companion page 298)
- Define myogenic contraction.
- Outline the role of cells in the sinoatrial node.
The contraction of the heart is myogenic. This means that the signal for cardiac compression arises within the heart tissue itself. In other words, the signal for a heartbeat is initiated by the heart muscle cells (cardiomyocytes) rather than from the brain:
- Membrane of the heart muscle cell depolarizes when the cell contracts, which then activates the adjacent cells so they contract
- Sinoatrial node: Group of small special muscle cells in the wall of the right atrium that beats at the fastest rate
- Cells have extensive membranes
- Sinoatrial node initiates each heartbeat because the cells depolarizes the first
6.2.U9 The sinoatrial node acts as a pacemaker. (Oxford Biology Course Companion page 299)
- State the reason why the sinoatrial node is often called the pacemaker.
Within the wall of the right atrium are a specialised cluster of cardiomyocytes which direct the contraction of heart muscle tissue.
This cluster of cells are collectively called the sinoatrial node (SA node or SAN) sinoatrial node acts as a pacemaker. If defective, the sinoatrial node might be replaced by an artificial pacemaker
This cluster of cells are collectively called the sinoatrial node (SA node or SAN) sinoatrial node acts as a pacemaker. If defective, the sinoatrial node might be replaced by an artificial pacemaker
6.2.U10 The sinoatrial node sends out an electrical signal that stimulates contraction as it is propagated through the walls of the atria and then the walls of the ventricles. (Oxford Biology Course Companion page 299).Describe the propagation of the electrical signal from the sinoatrial node through the atria and ventricles.
The electrical conduction of a heart beat occurs according to the following events:
This sequence of events ensures there is a delay between atrial and ventricular contractions, resulting in two heart sounds - Lub Dub.
- Sinoatrial node initiates a heartbeat by contracting and sending out an electrical signal that spreads through the walls of the atria.
- Electrical signal can spread because there are connections between adjacent fibers across which allows for the signal to be spread.
- The spread of the electrical signal causes the left and right atria to contract.
- After 0.1 seconds, electrical signal is passed to the ventricles
- Time delay allows for atria to pump blood into the ventricles
- Blood is then pumped from ventricles into the artery
- This second node – the atrioventricular node (AV node) – sends signals down the septum via a nerve bundle (Bundle of His).
- The Bundle of His innervates nerve fibres (Purkinje fibres) in the ventricular wall, causing ventricular contraction.
This sequence of events ensures there is a delay between atrial and ventricular contractions, resulting in two heart sounds - Lub Dub.
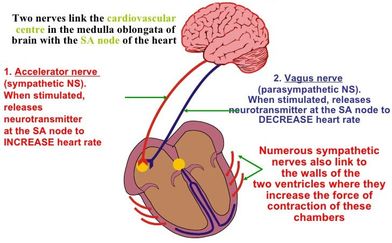
6.2.U11 The heart rate can be increased or decreased by impulses brought to the heart through two nerves from the medulla of the brain. (Oxford Biology Course Companion page 301)
- Outline the structures and functions of nervous tissue that can regulate heart rate.
- Describe factors that will increase heart rate.
- Describe factors that will decrease heart rate.
While the basal heart rate is determined within the heart by the pacemaker, it can be regulated by external signals.
- The rate of the pacemaker can be affected by nerves connected to the medulla region of the brain.
- Low blood pressure, high levels of CO2 (low pH) and low levels of oxygen, stimulate the heart to increase its rate and therefore deliver more oxygen to the tissues and remove more carbon dioxide
- High blood pressure, low levels of CO2 (high pH) and high levels of oxygen, cause the heartrate to slow down.
- Cardiac nerves which are part of the sympathetic nervous system cause the heart rate to increase.
- The Vagus nerve that is part of the parasympathetic nervous system causes the heart rate to slow down
- The medulla of the brain controls most of the autonomic functions of the body such as breathing, heart rate and blood pressure.
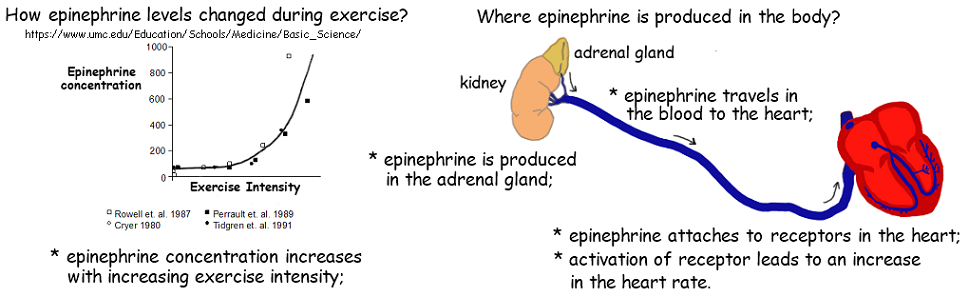
6.1.U12 Epinephrine increases the heart rate to prepare for vigorous physical activity (Oxford Biology Course Companion page 302
- Outline conditions that will lead to epinephrine secretion.
- Explain the effect of epinephrine on heart rate.
Hormones are chemical messengers released into the bloodstream that act specifically on distant target sites (like the heart). Heart rate can undergo a sustained increase in response to hormonal signalling in order to prepare for vigorous physical activity
- Cardiac nerves also cause the release of norepinephrine (adrenalin) from the adrenal glands during strenuous physical activity or times of high levels of stress. This is also known as the fight or flight response
- The Vagus nerve causes the heart rate to slow down through the release of acetylcholine, which has an inhibitory action on the heartrate
Application
6.2.A1 William Harvey’s discovery of the circulation of the blood with the heart acting as the pump. (Oxford Biology Course Companion page 304)
- Outline William Harvey’s role in discovery of blood circulation.
How the blood circulates around our body was discovered in the seventeenth century by a man named William Harvey. Click on the picture to get some background on Harvey.
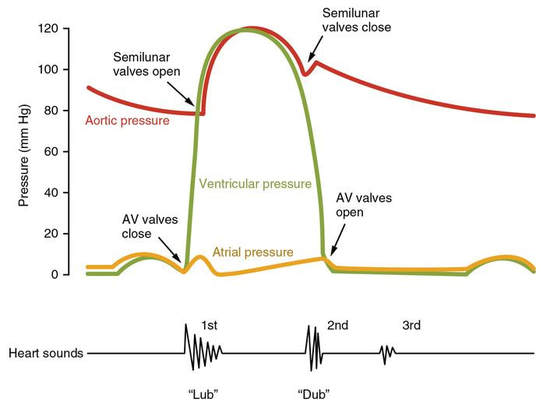
6.2.A2 Pressure changes in the left atrium, left ventricle and aorta during the cardiac cycle.(Oxford Biology Course Companion page 297)
- Describe the cause and consequence of atherosclerosis.
- Outline the effect of a coronary occlusion on heart function.
The cardiac cycle describes the series of events that take place in the heart over the duration of a single heart beat
Atrial Systole (0 to 0.1 s)
Ventricular Systole (approx. 0.1 – 0.5 s)
Atrial and Ventricular Diastole (approx. 0.5 to 0.8)
Atrial Systole (0 to 0.1 s)
- Atria contract, pressure increases in the left and right atria, and the remaining blood is pumped into the ventricles (left atrium into left ventricle)
- Ventricle walls relaxed and therefore the pressure is low
- AV valves are open and semi-lunar valves are shut
Ventricular Systole (approx. 0.1 – 0.5 s)
- Ventricles contract and the pressure increases dramatically in the ventricles
- AV valves close (because of the pressure) preventing backflow and the semi-lunar valves open.
- Blood is pumped out of the left ventricle into the aorta through the left semi-lunar valve
- Pressure in the aorta increases
- Pressure falls in the atria
Atrial and Ventricular Diastole (approx. 0.5 to 0.8)
- Muscles in the walls of the ventricles and atria relax
- The semi-lunar valves close
- Since the pressure drops in the atria, blood flows into the left atrium from the pulmonary veins and into the right atrium via the vena cava
- AV valves also open as the pressure in the ventricles drops below the pressure in the atria and blood flows from the atria into the ventricles (left atrium into the left ventricle through the left AV valve)
- Pressure in the aorta drops but remains quite high throughout the cycle because of the elastic and muscle fibres in the walls
6.2.A3 Causes and consequences of occlusion of the coronary arteries. (Oxford Biology Course Companion page 690)
- Explain the pressure changes in the left atrium, left ventricle and aorta during the cardiac cycle.
- Explain the relationship between atrial and ventricular pressure and the opening and closing of heart valves.
- Explain the atrial, ventricular and arterial pressure changes as illustrated on a graph of pressure changes during the cardiac cycle.
- Identify the time of opening and closing of heart valves on a graph o f pressure changes during the cardiac cycle.
Blood vessels that deliver oxygen and nutrient rich blood to the cardiac muscle tissue of the heart to allow it to pump blood around the body are known as coronary arteries
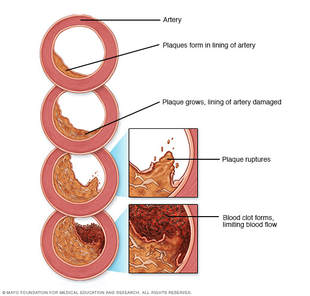
Causes
- Artery walls become damaged as fat (low-density lipoproteins) are deposited under the endothelium and fibrous tissue builds up
- Can result from a poor diet, over-eating, constant high blood glucose levels or smoking
- The flow of blood is impeded and the heart has to work harder to pump blood to the tissue, increasing blood pressure
- The smooth lining of the arteries begins to break down and form lesions called atherosclerotic plaques
- Platelets can bind to these lesions, causing an inflammatory response creating a blood clot
- The blood clot formed is called a thrombus and an embolus if it breaks free to travel through the bloodstream.
Consequences
- If an embolus breaks free, it can get stuck in a smaller arteriole and cause a blockage of blood supply to that tissue, eventually causing that tissue to die
- If this happens to the coronary arteries or arterioles in the heart, and enough of the tissue is deprived of oxygen, a myocardial infarction (heart attack) can occur
- If an embolus reaches the brain, and enough of the brain is deprived of oxygen and nutrients, a stroke can occur
- If coronary arteries are damaged, by-pass surgery can be performed, that takes an artery typically from a patient’s leg , replacing the damaged coronary artery
- Coronary Angioplasty (balloon angioplasty) can be an alternative to a by-pass operation. A catheter (with attached balloon) is inserted in the arm or the leg of a patient and is guided to the obstructed artery by x-ray and tv monitors
- A harmless dye is injected into the patient to determine exactly where is the blockage
- The balloon is inflated to reestablish blood flow stretching the arterial wall and squashing the plaques
Skill
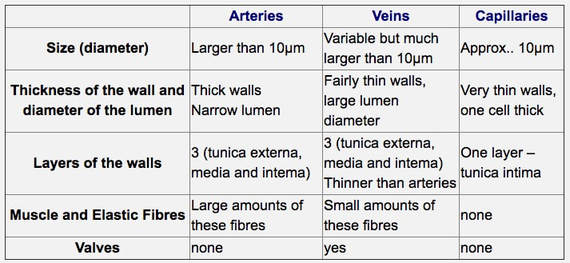
6.2.S1 Identification of blood vessels as arteries, capillaries or veins from the structure of their walls. (Oxford Biology Course Companion page 294).
- Compare the diameter, relative wall thickness, lumen diameter, number of wall layers, abundance of muscle and elastic fibres and presence of valves in arteries, capillaries and veins.
- Given a micrograph, identify a blood vessel as an artery, capillary or vein.
6.2.S2 Recognition of the chambers and valves of the heart and the blood vessels connected to it in dissected hearts or in diagrams of heart structure. (Oxford Biology Course Companion page 295).
- Label a diagram of the heart with the following structure names: superior vena cava, inferior vena cava, pulmonary semilunar valve, aorta, pulmonary artery, pulmonary veins, aortic semilunar valve, left atrioventricular valve, left ventricle, septum, right ventricle, left atrium, right atrium and right atrioventricular valve.
Key Terms:
|
vena cava
chambers nutrients superior venule oxygenated systemic circulation medulla capillaries hormones cardiac muscle vasoconstriction pocket valve atherosclerosis |
vessel
vena cava inferior vein deoxygenated coronary arteries cardiac nerve capillary bed carbon dioxide indefatigable vasodilation double pump cardiac cycle |
diffusion
valve atrium aorta artery semilunar valve sinoatrial node vagus smooth muscle Purkinje fibres pacemaker lumen diastolic |
blood
artrioventricular valve pulmonary artery pulmonary vein pulmonary circulation atrioventricular node adrenaline autonomic nervous system coronary occlusion systolic gravity muscle pressure skeletal muscle pressure double circulation myogenic contraction |
oxygen
ventricle arteriole circulation RBC myogenic CHD plasma oxygen heat epinephrine William Harvey micrograph |
Class Materials:
Tour the Heart
The Beat Goes On (ppt)
The Heart notes
Control of Heart Beat
Heart and Beat Diagram
Study Sheet For Circulatory Systen
Composition of Blood (worksheet)
Topic 6.2 Review
Tour the Heart
The Beat Goes On (ppt)
The Heart notes
Control of Heart Beat
Heart and Beat Diagram
Study Sheet For Circulatory Systen
Composition of Blood (worksheet)
Topic 6.2 Review
PowerPoint and Notes on Topic 6.2 by Chris Payne
Your browser does not support viewing this document. Click here to download the document.
Your browser does not support viewing this document. Click here to download the document.
Correct use of terminology is a key skill in Biology. It is essential to use key terms correctly when communicating your understanding, particularly in assessments. Use the quizlet flashcards or other tools such as learn, scatter, space race, speller and test to help you master the vocabulary.
External Links:
Circulation Overview
The Cardiac Cycle
Hyper Heart animation and graphs from University of Utah
Biointeractive from the Howard Hughes Medical Institute
Heart structure from FreezeRayPH School BioCoach – Cardiac Cycle
Can you explain why the flow of blood around the body is known as a double circulation?
Control of the Heart Beat
PH School BioCoach – Control of the Heart Beat
McGraw Hill: Conducting system of the heart
But does a heart actually need to ‘beat’? Well yes, if it is living. But not this rotor-based artificial heart.
Think about how fight-or-flight or exercise lead to a change in heart rate. Can you draw a flow-chart
Why not have a go at open heart surgery from abc.net.
HPD Link: Atherosclerosis and Coronary Heart Disease:
Medmovie has good animations for atherosclerosis, heart attacks and heart bypass surgery. Not in the SL syllabus, but a useful topic for life
Learn how to give CPR
In the News:
Eating breakfast (meal timing) lowers heart disease risk by more than twenty-five percent from Natural News
Massive DNA study points to new heart drug targets and a key role for triglycerides from Biology News
Researchers create nanopatch for the heart from Biology News
TOK
- Our current understanding is that emotions are the product of activity in the brain rather than the heart. Is knowledge based on science more valid than knowledge based on intuition?
Video Clips:
Now that we've discussed blood, we're beginning our look at how it gets around your body. Today Hank explains your blood vessels and their basic three-layer structure of your blood vessels. We're also going over how those structures differ slightly in different types of vessels. We will also follow the flow of blood from your heart to capillaries in your right thumb, and all the way back to your heart again.
Great video clip on the SA and AV nodes of the heart from McGraw Hill
Drawing an IB Heart
Hank takes us on a trip around the body - we follow the circulatory and respiratory systems as they deliver oxygen and remove carbon dioxide from cells, and help make it possible for our bodies to function.
Paul Andersen surveys the circulatory system in humans. He begins with a short discussion of open and closed circulatory systems and 2,3, and 4-chambered hearts. He describes the movement of blood through the human heart and the blood vessels. He discusses the major components of blood and the cause of a heart attack.
For most of history, scientists weren't quite sure why our hearts were beating or even what purpose they served. Eventually, we realized that these thumping organs serve the vital task of pumping clean blood throughout the body. But how
How adrenaline and acetylcholine affect heart rate
Approximately seven million people around the world die from heart attacks every year. And cardiovascular disease, which causes heart attacks and other problems like strokes, is the world’s leading killer. So what causes a heart attack?
Hemophilia - Watch this digital animation, specifically developed by biotherapeutics leader CSL Behring for kids and/or caregivers of newly diagnosed patients with hemophilia A or hemophilia B, to learn more.